This is Part I, Case 1 in a series of cases that I completed, documented, and submitted for dental implant credentialing exams. I strongly believe in the value of credentialing exams to learn from a group of likeminded dentists, showcase your own knowledge to your staff, patients, and colleagues, and help promote quality dental implant care in the dental community.
I hope that sharing these case reviews will help others prepare for the AAID/ABOI Oral Exams and Case Presentations as well as showcase a good variety of implant cases to learn from. The posts will mimic the exact template of submitted cases for their respective exams. The breakdown of cases for this series will be spread out over the next several months but here is an outline of cases to look forward to reviewing:
- Part 1: AAID (American Academy of Implant Dentistry) Associate Fellow Exam
- Case 1: Single Tooth Implant
- Case 2: Quadrant Implant Case
- Case 3: Full Arch Implant Case
- Part 2: ABOI (American Board of Oral Implantology) Diplomate Credentialing Exam
- Case 1: Implant Overdenture
- Case 2: Lateral Sinus Lift and 2 Implants
- Case 3: Single Implant in the Esthetic Zone
- Case 4: Immediate Implant
- Case 5: Fixed Full Arch All-on-X
- Case 5: Edentulous Quadrant with 2 or more implants
- Case 7: Horizontal Ridge Augmentation and 2 Implants
- Case 8: Candidate Choice (Guided Overdenture)
The Case
History
Patient presented as a 24 year old caucasian female with non-contributory medical history. Patient takes a daily multivitamin but otherwise has no known dental allergies, systemic diseases, or daily medications. She arrives presenting with a missing lower right first molar for 7 years. Patient’s chief concern is lack of prophylactic dental care for seven years since her lower right first molar was extracted, old silver fillings, cracked fillings, and a filling that has “fallen out” in the upper right second premolar.
Clinical Evaluation


Patient presents with all missing third molars and a missing lower right first molar. Minor crowding in anterior mandible and minor diastemas distal to bilateral peg laterals on maxillary arch. Patient has several amalgam restorations in the upper right first molar and second premolar, upper left premolars, and lower left first molar. Patient has a class I bilateral posterior occlusion and bilateral anterior class I occlusion. Periodontal probing was all within normal limits (<3 mm) except on the distal lingual of the lower left first molar where a 4mm pocket was noted. Patient reports no TMD symptoms. Edentulous site for the lower first molar was noted to have minor keratinized tissue width loss and minor ridge width loss due to partial edentulism.
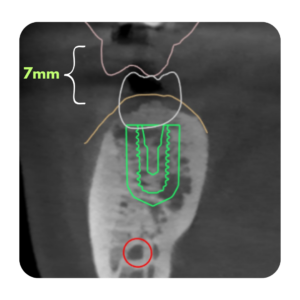
Patient is healthy periodontally and presents with several failing amalgam restorations and an asymptomatic necrotic lower left first molar. Patient has minor crowding in the anterior mandible but it is not a concern of the patients or contraindication to treatment. Patient presents with normal TMJ function, bilateral class I occlusion in posterior and anterior. The edentulous site for the lower right first molar exhibits minor to moderate soft tissue and hard tissue horizontal deficiency. Panoramic radiographs note that the inferior alveolar neurovascular bundle is 12-14mm from the resorbed crest of the ridge in the edentulous site. Soft tissue will be managed at second stage uncovery.
Radiographic Evaluation

Four bitewing radiographs and a panoramic radiograph were exposed at patient’s initial visit. The lower left first molar was noted to have a periapical radiolucency that was asymptomatic to the patient. Upon vitality testing the tooth was determined to be necrotic. Numerous amalgam restorations were noted in radiographs, bone levels appear stable and within normal limits, minimal radiographic calculus noted. The edentulous site for the lower right first molar was noted to have roughly 12-14mm from crest of bone to inferior alveolar neurovascular bundle with some noted vertical bone height loss.
Diagnosis: Patient was diagnosed with partial edentulism in the lower right first molar site. Patient was diagnosed as periodontally healthy and ASA 1
Treatment Plan: Patients chief concern was the missing lower right first molar and she was interested in dental implant therapy to regain the functional chewing of the right side. After clinical and radiographic exam it was proposed to place a root form dental implant in the edentulous site to restore the patients arch in the lower right first molar. Implant surgery was prosthetically driven to provide patient with screw-retained hybrid abutment porcelain implant crown. The lack of cement reduces the likelihood of peri-implantitis due to cement sepsis and allows for the simple retrieval of the restoration if necessary.
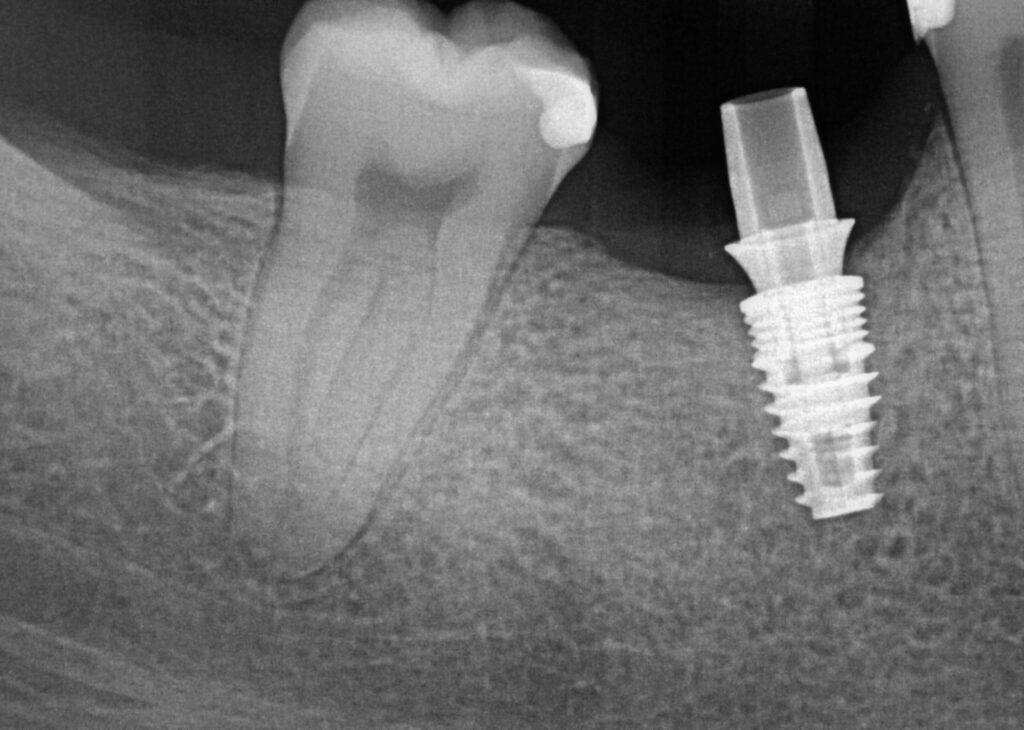
A 4.3x8mm BlueSkyBio Bio|Max implant was chosen. The implant has an internal conical connection with a 3.0mm platform switch. The 8mm length was chosen to allow for 1mm subcrestal placement while still leaving 3-4mm of bone between the implant apex and the inferior alveolar nerve. the 4.3mm diameter was determine at the surgical visit to allow for 1.5mm of thickness of bone on both buccal and lingual of the implant body for adequate healing and blood supply.
Surgical Notes:
Patient presented for dental implant surgery for the edentulous lower right first molar site. Patient confirmed that she had taken 2g of Amoxicillin 1 hour prior to her appointment. 3/4 carpule of 4% septocaine 1:100k epi was deposited in the buccal vestibule beneath the lower right second molar and the lower right second premolar. 1/4 carpule of 4% septocaine 1:100k epi was deposited at the mucogingival junction in the lingual tissue around the edentulous site.
A full thickness mucoperiosteal flap was raised with the incision splitted the keratinized tissue with 3mm buccal to the incision line. Bone width was verified with a perio probe and implant site was chosen midway between the lower right second premolar and second molar. Bucco-lingually the osteotomy was positioned to ensure 1.5mm of bone on the buccal of the final implant diameter.
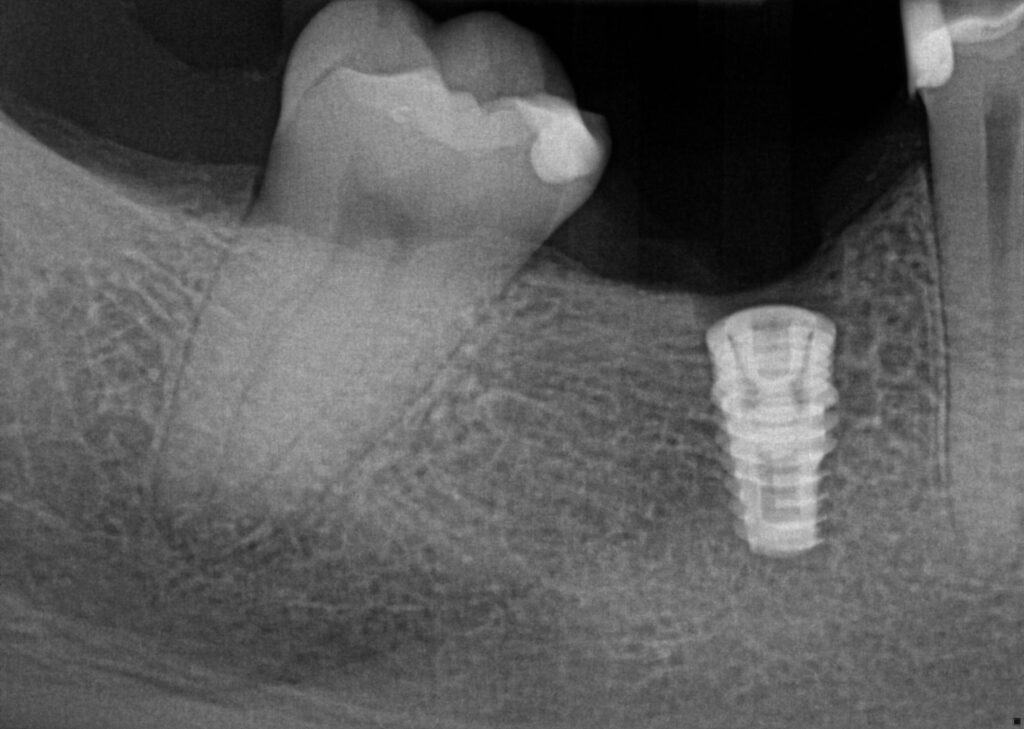
A pilot 2.0mm drill and subsequent osteotomy drills were drilled to depth of 9mm from the crest of the ridge to a width of 3.8mm. Osteotomy was verified to not have any fenestrations, dehisence, or perforations with a periodontal probe and flushed with 0.12% chlorhexidine gluconate solution.
a 4.3x8mm Biomax implant was placed with the implant handpiece until it reached a maximum torque of 32Ncm at which point the implant was driven the final 2mm with a hand wrench and implant driver. The implant was placed with a flat edge of an internal anti-rotational hex tangent to the buccal and 1 mm subcrestal. The implany body was flushed with 0.12% chlorhexidine gluconate solution and a cover screw inserted. The flap was replaced and primarily closed with three interuppted 3-0 PTFE sutures. Post-op instructions were given to the patient orally and in written form. Patient recommended to take 600mg ibuprofen for q6h for 2 days. Patient was seen 10 days later for post op visit and suture removal and noted that she had no discomfort. Sutures were removed and patient scheduled for future uncovery visit.
Prosthetic Procedures:
After 3.5 months of healing the patient returned for second stage uncovery. The incision was designed to be lingual line angle to lingual line angle of the lower right second premolar and second molar for a full thickness mucoperiosteal flap. Implant platform was exposed and cover screw removed. Implant body and surgical site flushed with 0.12% chlorhexidine gluconate. A 5mm tall wide permucosal abutment was placed and the buccal flap was positioned buccal to the healing abutment to regain lost soft tissue width. Two interupted chromic gut 4-0 sutures today to lightly hold flap in place. Patient instructed to swish with salt water twice a day for three days to keep site clean.
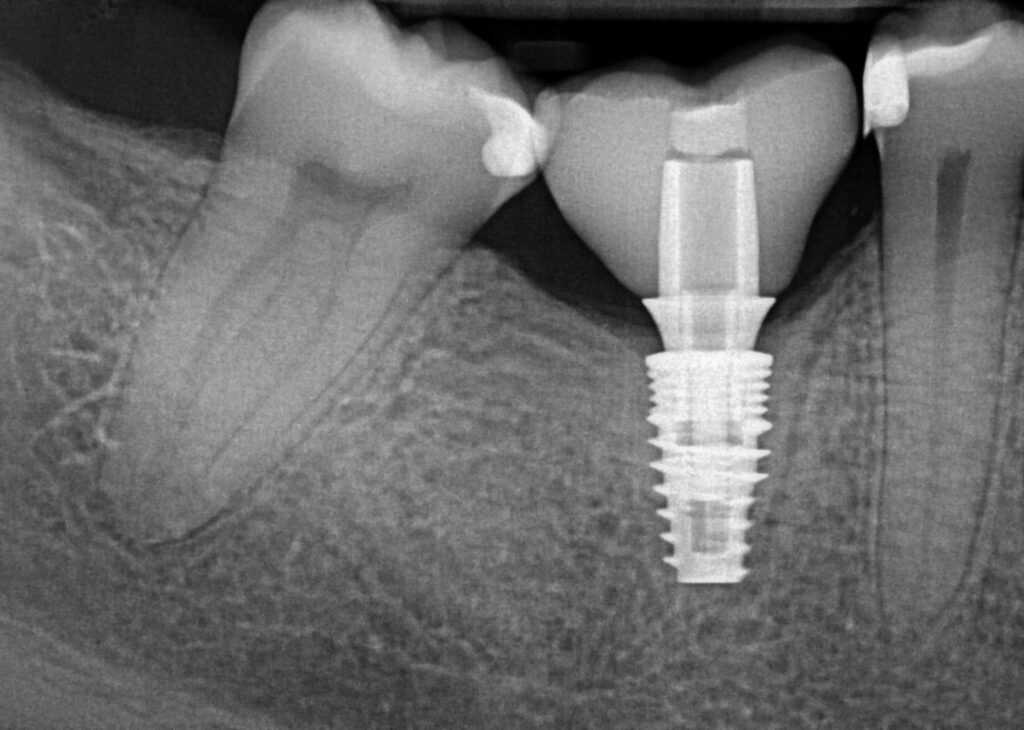
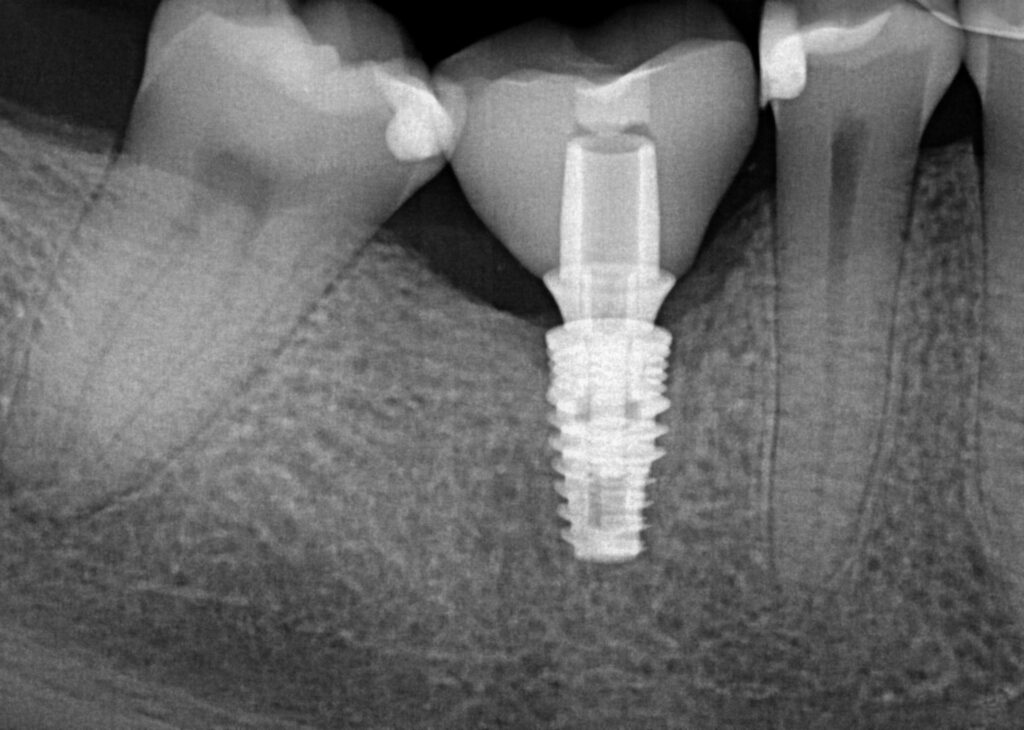
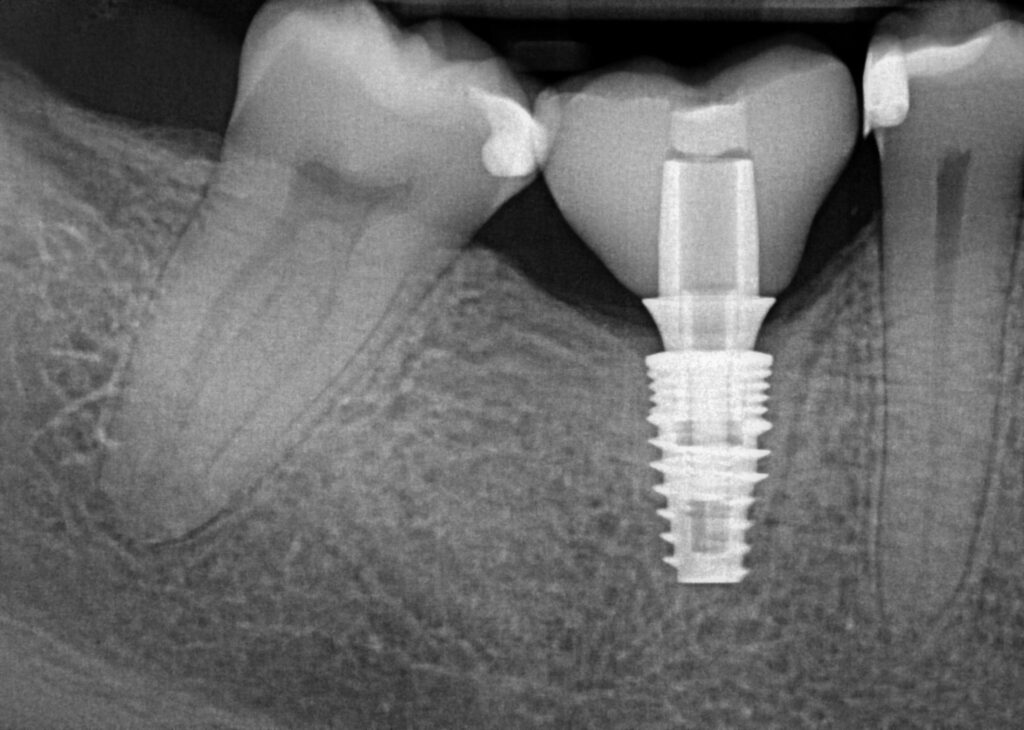
2 weeks after second stage uncovery visit the patient returned for digital final impressions. The healing abutment was removed and a gingival mask scan was taken of the lower right quadrant to capture the healed soft tissue contours. Opposing arch was scanned and the bite on the right side was captured with Sirona Cerec Bluecam and Cerec software. A 1.8mm collar height titanium base was placed in the implant platform and a Sirona scanbody placed. Cerec Bluecam scanning protocol to capture the final position of the implant for final prosthetics. Reinserted the healing abutment while designing final hybrid abutment and crown. A screw-retained Emax crown was designed and milled chairside with the Sirona MCXL mill and Ivoclar ceramic oven protocol. Final Emax (Lithium disilicate) crown was cemented with hybrid abutment cement from Rely X extraorally. Once cement was set and margins confirmed and polished the final screw retained crown was placed in the mouth. Contacts and full seating confirmed via floss and radiographs. The final crown was torqued to 30Ncm per manufacturers recommendations and occlusion was verified using articulating paper in maximum intercuspation and all excursives. Confirmed mild occlusion in maximum intercuspation with no excursive interferences.




Let me know what you think of these clinical credentialing cases in the comments! Hopefully this helps showcase a variety of implant case types and the documentation necessary for submitting cases for credentialing exams!




Responses
This is interesting dude, is this how you have to submit cases in order to get boarded?
Yeah they have very specific templates and guidelines for what to submit! ABOI requires 10 case presentations, a written 200 question exam, and an oral board exam. AAID is less strenuous but is the stepping stone towards board certification
Did you complete your credentialing process already? It would be cool to hear about your journey.
Yes I received my diplomate in the ABOI in 2021!
@vorholtdds bump